Diffuse idiopathic skeletal hyperostosis is associated with greater complexity of coronary artery disease burden on coronary angiography
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
Objective. Diffuse idiopathic skeletal hyperostosis (DISH) is a common disorder characterized by ossification of tendons and ligaments. DISH has been largely associated with an increased risk of metabolic syndrome and type 2 diabetes. The objective of the present study is to investigate the role of DISH in the risk of coronary artery disease (CAD).
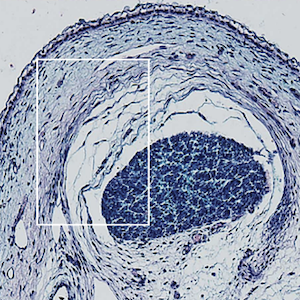
Methods. We conducted an observational cross-sectional study of patients without a history of rheumatic musculoskeletal diseases who underwent coronary angiography between March 2016 and April 2021. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score was calculated based on coronary angiography images. DISH diagnosis was based on standard X-ray images and computed tomography scans (Resnick criteria). Demographic and clinical characteristics were retrieved from electronic medical records. Multinomial and binary logistic regression models were employed to determine the association between SYNTAX score (dependent variable) and DISH (independent variable).
Results. The study included 187 patients, 82.9% of whom were men, with valid radiological imaging. 83 (44.4%) patients had a confirmed radiological diagnosis of DISH. Diagnosis of DISH was associated with a higher SYNTAX score [adjusted odds ratio (aOR) 34.1, 95% confidence interval (CI) 1.41-79.2 p=0.049], independently from traditional cardiovascular risk factors. In patients aged <70 years, DISH was associated with a 7-fold higher risk of belonging to the highest category of SYNTAX (≥34), compared to non-DISH (aOR 7.23, 95% CI 1.08-48.4; p=0.041). The extension of vertebral calcification was significantly associated with SYNTAX score (r2 0.378, p<0.0001).
Conclusions. DISH diagnosis is common in patients at high risk of cardiovascular disease or with definitive CAD. DISH was independently associated with higher CAD complexity.

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.