Comparison of clinicodemographic characteristics and pattern of vascular involvement in 126 patients with Takayasu arteritis: a report from Iran and Turkey
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
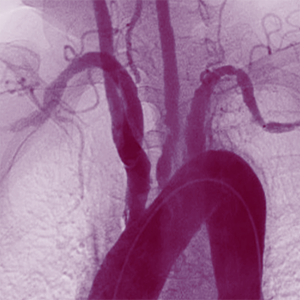
Takayasu arteritis (TA) is an extremely uncommon vasculitis that primarily affects the aorta and its branches. Due to the genetic and ethnicity effect, a diverse array of TA clinical manifestations has been reported worldwide. The purpose of the present study was to compare the clinicodemographic characteristics and pattern of vascular involvement of Iranian and Turkish TA patients. This study was a retrospective, cross-sectional investigation of 126 TA patients in Iran and Turkey. All of the variables analyzed were extracted from historical medical records. In 126 TA patients, the ratio of females to males was 8.6:1, and the average age at onset of disease was 30.5±11.1 years. Fatigue (49.2%) and a weak or absent pulse (79.4%) were the most prevalent symptoms and signs, respectively. The most prevalent angiographic classifications were types V and I in Iranian patients (41.09%) and type I in the Turkish population (47.7%) The left subclavian artery was the vessel most frequently affected by TA (66.6%). Our findings indicated that there were no significant differences between the two countries in terms of clinicodemographic characteristics or vascular involvement. Some clinical manifestations, such as claudication, were more prevalent in the Turkish population due to a higher incidence of occlusive lesions in the right subclavian artery.

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.










