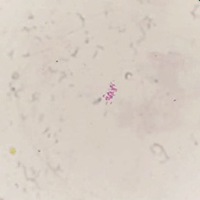
Multisystemic inflammatory syndrome related to COVID-19, with latent tuberculosis in bone marrow, and satisfactory response to tocilizumab, in a 7-year-old boy
Submitted: 15 August 2021
Accepted: 11 November 2021
Published: 7 February 2022
Accepted: 11 November 2021
Abstract Views: 5940
PDF: 626
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- G. Castellino, A. Protti, B. Canesi, Multiple Sclerosis and autoimmune diseases: clinical cases and review of the literature , Reumatismo: Vol. 53 No. 3 (2001)
- S. Capellino, P. Montagna, B. Villaggio, M. Cutolo, Effects of estrogen peripheral metabolism in rheumatoid arthritis , Reumatismo: Vol. 57 No. 2 (2005)
- M. Zoppi, M. Maresca, Symptoms accompanying fibromyalgia , Reumatismo: Vol. 60 No. 3 (2008)
- D. Jain, H.K. Aggarwal, V. Kaverappa, S. Dhayia, P. Jain, S. Yadav, Anti-dsDNA negative and anti-Ro positive lupus nephritis: a report of a rare case , Reumatismo: Vol. 65 No. 6 (2013)
- A. Murgo, E. Paresce, F. Fantini, Arthroscopic synovectomy in chronic inflammatory rheumatism: clinical and functional aspects , Reumatismo: Vol. 55 No. 1 (2003)
- P. Marson, G. Zanchin, C. Stefanutti, Some historical considerations on the inflammatory theory of atherosclerosis , Reumatismo: Vol. 56 No. 3 (2004)
- F. Atzeni, S. Sallì, M. Benucci, M. Di Franco, R. Casale, A. Alciati, P. Sarzi-Puttini, Fibromyalgia and arthritides , Reumatismo: Vol. 64 No. 4 (2012)
- G. Besutti, C. Marvisi, F. Muratore, L. Spaggiari, The role of sacro-iliac joint magnetic resonance imaging in the diagnosis of axial spondyloarthritis: focus on differential diagnosis in women , Reumatismo: Vol. 76 No. 3 (2024)
- S. Stisi, M. Cazzola, D. Buskila, M. Spath, M.A. Giamberardino, P. Sarzi-Puttini, G. Arioli, A. Alciati, G. Leardini, R. Gorla, M. Marsico, F. Ceccherelli, L. Bazzichi, R. Carignola, R.H. Gracely, F. Salaffi, L. Altomonte, F. Atzeni, Etiopathogenetic mechanisms of fibromyalgia syndrome , Reumatismo: Vol. 60 No. s1 (2008)
- M. Manara, M. Varenna, A clinical overview of bone marrow edema , Reumatismo: Vol. 66 No. 2 (2014)
<< < 9 10 11 12 13 14 15 16 17 18 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/reumatismo.2021.1448
https://doi.org/10.4081/reumatismo.2021.1448




