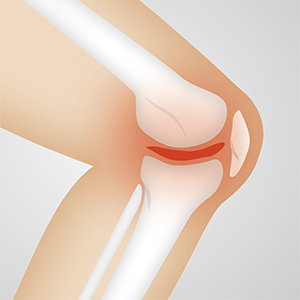
Magnetic resonance imaging as a structural refinement to the American College of Rheumathology clinical classification criteria for knee osteoarthritis
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
Objective: To evaluate if fulfilment of the definition of osteoarthritis (OA) based on the American College of Rheumatology (ACR) clinical criteria corresponds to pathological knee findings evaluated by magnetic resonance imaging (MRI). To evaluate if any such criteria is associated with a specific MRI pattern.
Methods: Forty-six consecutive patients aged 50 years or more referred by their general practitioners (GPs) to a radiology department because of non-traumatic knee pain underwent MRI using a dedicated low field (0.2 T) machine.
Results: MRI results were compared against the ACR criteria for knee OA. Patients with knee pain fulfilling the ACR criteria showed more severe synovial fluid effusion (OR 6.2, 95% CI 2.02 to 19.1), cartilage lesions in the medial area (OR 2.4, 95% CI 1.2 to 5) and higher mean number of osteophytes (OR 2.3, 95% CI 1.1 to 4.5). The association between single criteria and MRI features was more difficult to establish. Nonetheless, crepitus at joint movement was associated with synovial fluid effusion (p=0.02); bone enlargement was more frequent in patients with lesions of the posterior cruciate ligament (p=0.0001); no palpable warmth was associated with cartilage lesions (p=0.02), and morning stiffness shorter than 30 minutes was associated with the surface of bone edema (p=0.02).
Conclusions: The ACR clinical criteria identify patients showing the most important features of OA. The association between individual clinical ACR criteria and OA pathology depicted by MRI may be difficult to explain on the basis of anatomical changes and needs further evaluation.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.