Multisystemic inflammatory syndrome related to COVID-19, with latent tuberculosis in bone marrow, and satisfactory response to tocilizumab, in a 7-year-old boy
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
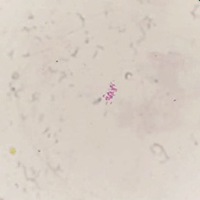
Paediatric inflammatory multisystem syndrome temporally associated with COVID-19 (PIMS-TS) or multisystem inflammatory syndrome in children (MIS-C) is a new acute-onset systemic inflammatory disease, which mainly affects children. Latent tuberculosis infection (LTBI) is characterized by the presence of immune sensitization to Mycobacterium tuberculosis (MTB) in the absence of any clinical or radiological evidence of active disease. We present a child with MIS-C related to COVID-19, with latent TB in the bone marrow, and satisfactory response to tocilizumab. It is important to pay attention in the investigation of TB cases in countries with a high prevalence of tuberculosis, especially when opting for immunusuppression.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.