Successful treatment of COVID-19 induced neutrophilic myositis with intravenous immunoglobulin and corticosteroids: a case report
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
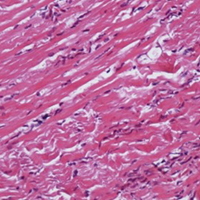
Neutrophilic myositis (NM) is an inflammatory disorder predominantly characterized by neutrophilic infiltration in the muscles, which is suggested to be an extracutaneous manifestation of neutrophilic dermatosis (ND). NM is a rare disorder which has been occasionally reported in association with hematologic and inflammatory disorders. This case report describes a 45-year-old woman who presented with gradual muscle weakness developed after coronavirus disease 2019 (COVID-19) infection. Electromyography and nerve conduction velocity findings were compatible with inflammatory myopathy and muscle biopsy revealed neutrophilic infiltration. She was successfully treated with intravenous immunoglobulin, prednisolone 1 mg/kg/day and azathioprine 150 mg/day. In conclusion, the COVID-19 infection itself and the drugs used to treat it can cause a number of muscle disorders. Awareness of muscular involvement in COVID-19 infected patients is important for early diagnosis and appropriate treatment.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.